Just putting one where the last cardiac arrest occurred isn’t optimal — more calculations to get to fewer steps
Sudden cardiac arrest, which occurs when the heart unexpectedly stops beating, kills more than 400,000 people in the U.S. and Canada every year. Death happens within minutes if not treated, and 92 percent who suffer an attack outside of a hospital don’t survive.
The use of automated external defibrillators, or AEDs, which deliver a strong electric shock to jolt the heart back into action, can dramatically improve survival rates. But the key is quick action; the American Heart Association says that when defibrillation is applied within five minutes, the survival rate can be as high as 45 percent. The units can cost about $3,000 each. An industry estimate puts the number of AEDs in the U.S. at 2.4 million.
Because AEDs can be used by untrained bystanders, health officials want to see them widely deployed in workplaces, malls, restaurants, subway stations and other public places. Research has found that access to AEDs drastically reduces the delay in treating cardiac patients. One estimate suggests that widespread deployment of defibrillators could save as many as an additional 4,000 lives per year in the U.S.
Opt In to the Review Monthly Email Update.
The trouble is, AEDs are rarely used. There are lots of reasons, but one is that the devices aren’t always located where they can be reached quickly in an emergency.
That’s the problem tackled by University of Toronto’s Timothy C.Y. Chan, UC Berkeley’s Zuo-Jun (Max) Shen and UCLA Anderson’s Auyon Siddiq in a paper published in Operations Research. The authors propose a model for deploying publicly accessible AEDs where they’re most likely to be used by taking into account where cardiac arrests might occur, not just where they happened in the past. With the model, the authors say, health officials can position the devices in a way that “can improve survival rates by shortening the distance to the nearest AED.”
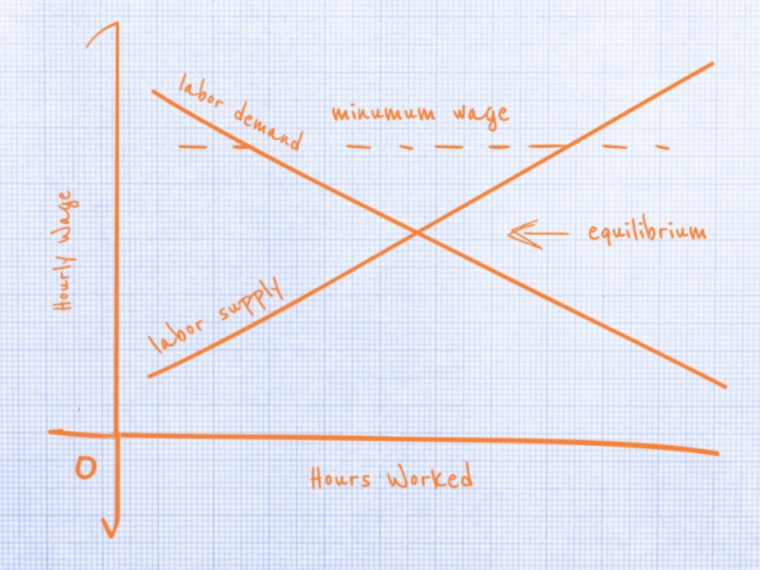
Typically, AEDs are placed where people congregate, such as shopping malls or office buildings, but these aren’t always easily accessible when an attack occurs out on the street. Researchers have tried to improve the availability of AEDs by looking at the site of previous attacks. But given the random nature of cardiac arrests, this method fails to consider where they could take place in the future. Another approach is to estimate the number of incidents that occur within a certain distance of an AED location. This can make the devices accessible to the average patient, but can leave many victims dangerously distant from the nearest device.
With their model, Chan, Shen and Siddiq seek to improve on existing methods by addressing the uncertainty about where cardiac arrests might occur in the future and by making sure the most distant victims are still near an AED.
Normally, modeling all the possible locations would be a computational nightmare. The authors devised an efficient way to solve the problem by considering only a subset of the millions of alternatives. This, the research suggests, is enough to come up with a model that performs better than one that bases siting decisions on the location of past cardiac arrests.
The authors considered the problem of deploying 30 AEDs in Toronto’s densely populated financial district. They mapped the 43 cardiac arrest events that occurred in public areas from January 2006 to April 2013, and then identified 120 public places, such as restaurants or shops, where AEDs could be deployed. They divided the area into 15 equally shaped cells and, using their model, projected where cardiac arrests could occur. By comparing distances, they then determined the optimal placement of AEDs.
When compared with a model that used historical cardiac arrests, the authors’ model reduced the distance between an attack and the nearest AED by at least 9 percent on average and as much as 20 percent. Using Google Maps to measure walking distances, they estimated that with their model, cardiac arrests on average would occur 12 meters closer to the nearest AEDs than would those based on past attacks. For patients that were the most distant, the authors’ model placed devices 11 meters closer.
While the approach is largely theoretical, it shows that it’s possible to come up with a way to deploy AEDs that’s better than existing methods, the authors suggest. It could be especially effective when combined with a “crowdsourcing” approach to responding to cardiac emergencies. Mobile apps, such as an application developed by San Francisco-based PulsePoint Foundation, can be used when a cardiac arrest occurs to alert nearby volunteers and identify the nearest AED, potentially shaving crucial minutes off response times.
“In a setting where lay responders are recruited to intervene during a cardiac arrest,” the authors write, “it is even more critical that AEDs are tactically located throughout an urban area.”
Featured Faculty
-
Auyon Siddiq
Assistant Professor of Decisions, Operations and Technology Management
About the Research
Chan, T.C.Y., Shen, Z., & Siddiq, A. (2017). Robust defibrillator deployment under cardiac arrest location uncertainty via row-and-column generation. Operations Research, 66(2), 358–379. doi: 10.1287/opre.2017.1660