Getting the mix right is the goal of a Medicare pilot, which itself could use substantial improvement
Primary care is a universal pain point in the U.S.
Turned off by a system that offers greater financial incentives for specialists, too few medical students become internists or family medicine physicians. By one estimate, the best-case scenario is that in 10 years we will be short more than 20,000 primary care physicians needed to meet patient demand.
That’s already creating a traffic jam of anxiety and frustration. Patients clamor for too few appointment openings, and overloaded doctors are increasingly on the clock to finish one consult and quickly move on to the next, which, however inadvertently, may impact the quality of the interaction and the care.
Opt In to the Review Monthly Email Update.
Medicare has long experimented with how to improve the primary care experience for doctors, patients and taxpayers; it ran three different pilot programs from 2011 to 2017.
In a paper published in Manufacturing & Service Operations Management, UC-Riverside’s Elodie Adida and UCLA Anderson’s Fernanda Bravo examine a Medicare program launched in 2021, called Primary Care First, being test-run by about 900 primary care practices.
The PCF program mixes a per-patient capitation fee paid to doctors (upfront monthly payment for managing the care of each patient) with reduced fee-for-service payments regardless of whether a patient is seen remotely or in person. The current flat fee for service under PCF is $40.82. PCF also layers in an incentive program for practices that meet a baseline for delivering patient value (based on appointment wait time, management of chronic conditions and outcomes).
The researchers’ analysis finds that the PCF approach “can indeed drastically improve upon fee for service,” and they go on to offer some enhancements to make the program better still.
Adida and Bravo find that remote telehealth care works well for provider and patient when properly deployed. Yet, remote consults are not something Medicare has historically been on board with.
The Pandemic’s Remote Silver Lining
The Centers for Medicare & Medicaid Services has long resisted — not paid for — telehealth, out of concern about quality of care and privacy. All that changed with the onset of the pandemic. With a temporary green light from CMS, telehealth appointments increased tenfold — from about 5 million to 53 million — in the first nine months of the pandemic.
Adida and Bravo suggest Medicare should reimburse remote care and make it a permanent piece of primary care delivery, finding that it not only benefits physicians in terms of greater productivity — past research suggests tele appointments can take less than half as long as in-person appointments — but when properly used, also benefits the patient by reducing commute and wait times, without compromising health outcomes.
Using patient and provider data from 14 states that participated in a prior Medicare test program, Adida and Bravo built a model to explore the interplay between how doctors are paid and their patient outcomes under the PCF structure. (Actual PCF data will not be available until the first five-year wave is completed in 2026; a second wave will be complete in 2027.)
The incentive bonus for patient value can be as much as 50% of revenue derived from Medicare patients under the PCF program, though the study looks at an interim level of up to 34%. Failure to meet the service quality baseline triggers a 10% penalty, though, the researchers point out, given that the program is voluntary, it stands to reason that only practices confident they can meet the baseline will participate.
Depending on the patient complexity, Adida and Bravo analyzed how primary care doctors choose between remote care, in-person appointments or referrals to a specialist. While more granular data affects costs and care, these three main options — and apportioning patients appropriately among them, especially for the health profile of the population served — represent the biggest mechanism for managing the shortage of primary care capacity.
The researchers’ model explores the mix of care delivery options that would deliver the optimal solution of best compensating primary care doctors while also delivering the best possible quality of care for patients, which can reduce overall spending, benefiting taxpayers.
In their model, optimizing for both physicians and patients would entail doctors using remote care for the least complex patients and referring the most complex to specialists. The in-betweens would be seen in person by the primary care physician, with an average wait time that would qualify for the service quality bonus. Their model also calibrates for the increased health risk remote care may pose.
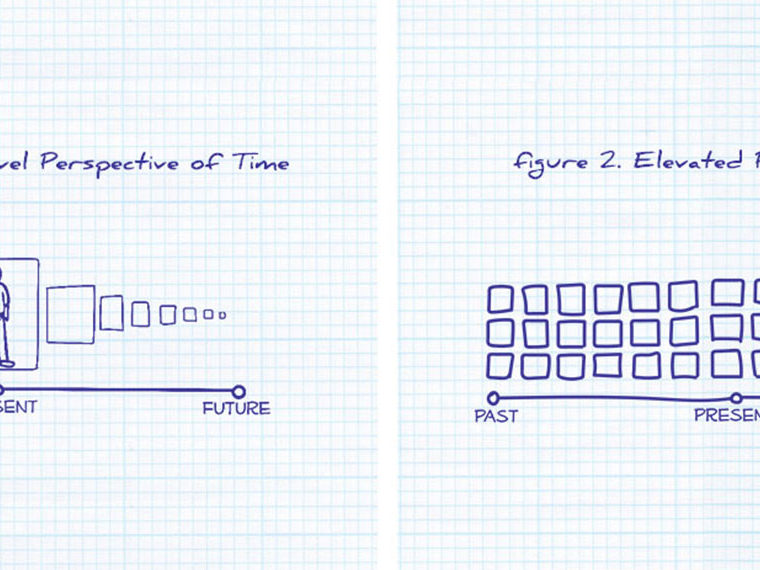
The chart below shows the current mix of care, based on a high capitation fee and based on patient complexity.
The red and blue dashed lines show the sweet spot for where in-person care should be utilized. To the left of the blue line would be optimal level of remote care, and to the right of the red line is the optimal level of specialty care.
The state-by-state variation reflects differences in the overall health level of a given state’s Medicare population (the less healthy a population, the more in-person care would be needed).
As you can see in the graphic, when doctors are paid a high capitation fee, it leads to significantly more — too many — referrals to specialists. That makes sense when you consider the primary care doctor has already been paid a higher capitation fee for having the patient, and by referring out treatment, the odds are increased for a better outcome, which helps earn the value bonus.
A key assumption the researchers make is that referrals also make it possible for primary care physicians to take on new patients, which they assume are not Medicare, thereby also increasing their revenue prospects. (That’s a fair assumption given 70% of the average primary care practice is private, not Medicare.)
Adida and Bravo find these major flaws in the PCF program:
- It sets primary care visit fees — in person or telehealth — nationally at about $40 and that’s too low for many markets.
- The program doesn’t result in enough telehealth visits, which thus strains primary care capacity with more time-consuming office visits and referrals to specialists.
- Overall, PCF results in too many referrals to specialists.
Thus, Adida and Bravo suggest any future program iteration should consider modifying the per-visit fee to reflect the general health of a given state’s Medicare population.
The 14 states studied are ranked below in descending order of health status of Medicare enrollees. For the states with lower overall health — Tennessee, Oklahoma and Ohio — the flat $40.82 in place today is close to the optimal fee, as denoted in the darker filled-in circle to the right. But in states with a healthier population and with less utilization of in-hospital care, such as Hawaii, Montana and Colorado, the researchers propose that a higher fee-for-service rate would incentivize primary care physicians to see more patients rather than quickly refer out to specialists.
The Waiting Game
Adida and Bravo also recommend that care should be taken in setting benchmarks for wait time. While patients may assume a short wait time should always be the goal, that can have an unintended consequence. The researchers note that a too-short wait-time benchmark compels primary care physicians to limit the use of in-person care for Medicare patients — seeing them either remotely or referring them to a specialist — and instead prioritize seeing new patients, who are not reimbursed under PCF, in the clinic. Anyone who lives in the world of copays can understand the added cost to patient (and taxpayer) of an over-reliance on specialty referrals.
As the largest single “payer” for medical services in the U.S., Medicare has plenty of incentive to pursue a health care delivery system that works best for primary care physicians, their patients and the taxpayers who shoulder a large part of the cost. This research suggests the quality-of-care bonus incentive structure of PCF works, but future program iterations should consider tweaking the reduced fee-for-service rate and the capitation payment to better align physician and patient outcomes based on a state’s overall health status.
Featured Faculty
-
Fernanda Bravo
Assistant Professor of Decisions, Operations and Technology Management
About the Research
Adida, E., Bravo, F. (2023). Primary Care First Initiative: Impact on care delivery and outcomes. Manufacturing & Service Operations Management.