That approach, closer to an opt-out, beat three nudges, or opt-ins at encouraging younger people to get tested
An alarming rise in colorectal cancer diagnoses for 40-somethings — it’s now the leading cause of death for men ages 45 to 49 and the second-leading cause for women in that age group, behind breast cancer — prompted a lower recommended age for screening to 45 from 50.
The two most common screening methods are a preventative colonoscopy or a fecal immunochemical test that analyzes stool. Both are covered by insurance. But uptake, since the 2021 change, falls short of screening levels achieved after decades of pushing those 50 and older to get screened. (These age recommendations are for people without a family history of colorectal cancer, it should be noted.)
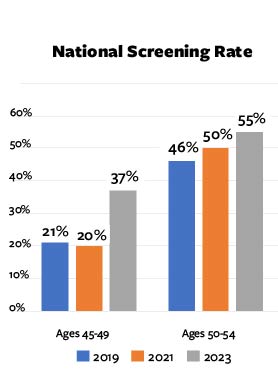
Getting to 37% screened from 20% in just two years was an impressive leap. Researchers, of course, want to further the progress.
A randomized clinical study involving more than 20,000 patients of the UCLA Health system set out to see if there might be a way to compel more 40-somethings to get tested. A team of 10 researchers, including UCLA Anderson’s Hengchen Dai and Craig Fox, randomly sorted the study population into four groups.
Three received “active choice” nudges, delivered via the electronic health care portal, that asked participants to explicitly indicate if they wanted to get tested or if they wanted to decline the screening offer. The fourth took the opt-out approach: A testing kit was proactively sent to the participants home, completely unsolicited. In addition, a message was delivered via the patient portal to the fourth group of patients, informing them that they could get screened and a testing kit was sent to them. For all groups of patients, the patient portal messages included contextual information on why screening was recommended.
Guess What Came in the Mail?
In the results, published in JAMA, the surprise testing kit was the winner.
Success was defined as the patient following through with either screening method within six months of receiving a notification on the digital health care portal that they could get screened.
Among patients who were sent a FIT test by default, 26% got screened within the six month window. Of those who got screened in this group, about two-thirds stuck with the FIT test and one-third instead got a colonoscopy.
Nearly 3 in 4 people who received the unsolicited FIT kit and whose stool sample triggered an abnormal result followed through with a colonoscopy within the six-month research window.
The 26% completion rate triggered by the proactive mailing of the at-home test kit was markedly higher than the active choice nudges:
- 16.4% of participants who were sent a digital notification asking them to choose between having a FIT kit sent to them and declining the offer completed a screening test.
- 14.5% who were asked to choose between scheduling a colonoscopy and declining the offer, chose to get tested.
- 17.4% who could choose getting a FIT kit, scheduling a colonoscopy or declining the screening offer completed a screening (among those who got tested within this group, about two-thirds chose a colonoscopy, one-third got screened via the FIT kit).
The difference in screening rates between people receiving the FIT kit by default and people invited to make an active choice held up regardless of race/ethnicity, income and health insurance status (private, Medicare, Medicaid, no insurance).
Opt-Out Vs. Active Choice
While opt-out nudges sometimes get blowback as being paternalistic, or anti-libertarian, this study suggests the method might save more lives than requests that require an active choice. It also dovetails with perhaps the biggest nudge success to date: When 401(k) plan sponsors stopped asking people if they wanted to participate in the retirement plan (opt-in) and automatically enrolled them in the plan (opt-out, with the option to leave at any time) enrollment jumped — and has stayed higher.
Of course, there’s not yet a way to send breast cancer and lung cancer tests to people’s physical mailboxes, but the relative success of the here’s-the-FIT-kit-you-didn’t-even-ask-for approach may work in other realms where nudges often bend over backward to not seem too pushy or offer choice to spur buy-in. At least for colon cancer screening for a newer universe of target patients, the takeaway was: No choice was better than some choice, and easiest was best.
In this colon screening field experiment, the large gap in the effectiveness of the opt-out option relative to the three active choice nudges, shows the value of continuing to study and refine what nudges may actually compel more of us to adopt behaviors that can help us.
Featured Faculty
-
Hengchen Dai
Associate Professor of Management and Organizations and Behavioral Decision Making
-
Craig Fox
Harold Williams Chair and Professor of Management
-
Maria Han
Chief Quality Officer for the UCLA Health Department of Medicine and Assistant Clinical Professor
-
Sitaram Vangala
David Geffen School of Medicine at UCLA
-
Folasade P. May
David Geffen School of Medicine, Associate Professor; UCLA Kaiser Permanente Center for Health Equity, Associate Director
About the Research
Galoosian, A., Dai, H., Croymans, D., Saccardo, S., Fox, C.R., Goshgarian, G., De Silva, S., Han,M., Vangala, S., & May, F.P. (2025). Population Health Colorectal Cancer Screening Strategies in Adults Aged 45 to 49 Years. JAMA, 334(9), 778-787.