Smartphone GPS tracks staffers between facilities
The deadly outbreak of the coronavirus at a Kirkland, Washington, nursing home in early March 2020 set off a nationwide scramble to better protect the vulnerable elderly. The U.S. Centers for Medicare & Medicaid Services (CMS), the federal regulator of nursing homes, promptly issued a new rule that restricted visitors from entering facilities.
What hasn’t been addressed is the mobility of nursing home caregivers, and how that is exacerbating virus breakouts. Not only are nursing home staff coming and going to their jobs, a significant portion are also working at more than one facility.
UCLA Anderson’s M. Keith Chen and Elisa F. Long, and Yale University’s Judith A. Chevalier find that workers who shuttle between different nursing homes are serving as spreaders. In a working paper, the researchers estimate that if workers had the incentive to stay put at one facility, outbreaks at nursing homes could be reduced by an estimated 44%. That would obviously have an impact on the alarming death toll at nursing homes. The CMS reports that more than 30% of nursing home residents in New Jersey, Connecticut and Massachusetts had contracted the virus through late June, and that nearly 10% of nursing home residents in those states had died.
Opt In to the Review Monthly Email Update.
The researchers provide empirical heft to what was well-known by major stakeholders. In March, just as CMS was putting nursing homes on lockdown, a report from the Centers for Disease Control and Prevention (CDC) mentioned care providers’ working at multiple locations as a likely source of virus spread. A study by New York State estimated that about one in four nursing home workers tested positive and thus were likely a main source of virus spread.
The culprit here is a system that effectively encourages (if not outright forces) workers to shuffle among multiple facilities. Many nursing homes rely on staffing services to deliver workers on a just-in-time/just-as-needed basis, rather than directly hire full-time staff. At a median hourly pay rate of $14.25, making a living wage can require patching together work at multiple facilities. Even then, the essential work of nurses’ aides and orderlies at skilled nursing facilities provides a median salary below $30,000, according to the Bureau of Labor Statistics.
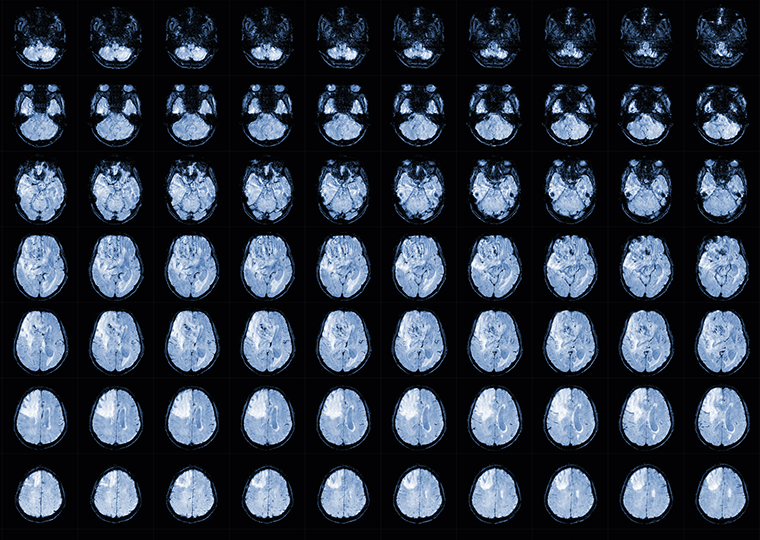
Chen, Chevalier and Long confirm the peripatetic nature of nursing home employment by tracking the geolocation data on nearly 510,000 smartphones that showed up inside more than 15,300 nursing homes in the continental U.S. This wasn’t an exercise in proximity to a cell tower. The anonymized data from Veraset tracked pings from inside nursing homes.
The data were collected for six weeks from the date that nursing homes were under lockdown (March 13, 2020), on the presumption that the only people (represented by smartphones) entering the facility would be caregivers and support staff such as hospice workers and dialysis technicians, as well as janitorial and food service providers.
The researchers found that 7% of individuals who entered one facility also showed up inside another facility. On average, they found, one facility is connected to 14 more by a traveling worker. In rural settings (Montana and Vermont, for example) the cross-facility job hopping was far more muted, with a smartphone showing up in fewer than two facilities. In Florida, Illinois, Maryland, New Jersey and Texas, a single smart phone was pinging from an average of 20 other facilities.
The researchers’ analysis estimates that expected COVID-19 cases at the most highly connected facility within a state is more than 190% higher than the expected outbreak at the least-connected facility.
“These results provide evidence of the magnitude of the benefits that would derive from compensating nursing home workers to work at only one home and limiting cross-traffic across homes,” write Chen, Chevalier and Long.
They also note that while the nursing home population is extremely vulnerable, the research suggests that a similar approach to other “congregate settings,” such as assisted living homes, prisons and food-processing plants, would likely help bend the outbreak curve down.
Featured Faculty
-
M. Keith Chen
Professor of Economics
-
Elisa Long
Associate Professor of Decisions, Operations, and Technology Management
About the Research
Chen, M.K., Chevalier, J.A., & Long, E.F. (2020). Nursing home staff networks and COVID-19.